In a striking revelation, three individuals linked to Evergreen Recovery, Inc., a drug and alcohol treatment center, have been implicated in an extensive Medicaid fraud and money laundering scheme that highlights the vulnerabilities in healthcare systems. Operating from March 2018 to July 2024, the scheme employed deceptive practices to manipulate Medicaid and other healthcare programs, fraudulently billing for services that were often never provided or did not qualify for reimbursement.
The Fraudulent Tactics Employed
Offering “Sober” Housing as a Ruse
Key tactics used by the defendants included offering free “sober” housing to clients under the condition they enroll in Evergreen Recovery’s programs. This allowed the defendants to systematically overbill Medicaid by coercing clients into attending unnecessary or non-existent sessions. They further recruited vulnerable individuals from homeless shelters, probation offices, and other treatment programs, threatening eviction and loss of their belongings if they missed any sessions.
By leveraging the promise of free housing, the defendants exploited the precarious circumstances of those in desperate need of recovery services. The coercion extended to unwarranted sessions ensured a steady influx of funds from Medicaid, which amplified the scale of the fraud. This not only manipulated the healthcare system but also victimized the very people seeking help by forcing their participation in a fraudulent cycle.
Fabricating Health Records for Profit
The investigation revealed that the defendants fabricated health records to inflate billing amounts, sometimes creating false entries long after the supposed treatment dates. Peer Coaches employed as part of the scheme were directed to falsify their client interaction records. This misconduct facilitated overbilling for services like group and one-on-one counseling and treatment coordination.
Implementing such fraudulent documentation tactics further evidenced the lengths to which the schemers went. By instructing employees to falsify records, they established a consistent method to justify excessive and unjustified billing. The exploitation of Medicaid through these fabricated records illustrates the systemic abuse within the organization, extending the criminal activity to multiple levels of the corporation.
Legal Consequences and Investigation Findings
Charges and Court Appearances
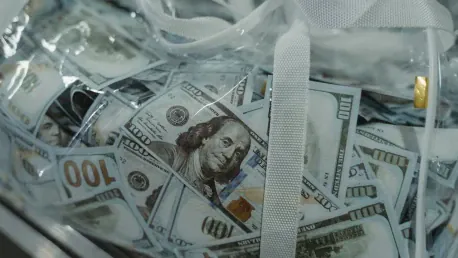
Facing serious charges, the three defendants have been indicted for conspiracy to commit wire fraud, wire fraud, and one additionally for money laundering, reflecting their use of ill-gotten gains for illegal financial transactions. Two of the defendants made initial court appearances on December 19, 2024, and were released with conditions barring contact with former clients or employees of Evergreen. The third is due in court on December 23, 2024.
These legal proceedings mark a significant step in holding the accused accountable for their actions. The court’s stipulations on communication restrictions highlight the severity of the case and the need to protect witnesses and victims from potential intimidation or retribution. The defendant’s use of ill-gotten funds not only signifies the extent of the financial misconduct but also underscores the broader implications of the fraud on public trust in healthcare programs.
Collaboration and Impact of the Investigation
The investigation, led by the FBI and the Health and Human Services – Office of Inspector General, with assistance from the Medicaid Fraud Control Unit, underscored the exploitation of programs intended to aid vulnerable populations. While the indictment underscores the suspected guilt of these individuals, it is essential to remember that they are presumed innocent until proven guilty.
The collaborative framework of this investigation highlights the importance of multi-agency efforts in tackling such complex and systemic fraud schemes. Bringing together federal and state resources facilitated a thorough examination of the scheme, ensuring that detailed evidence was gathered and analyzed. This comprehensive approach is critical in dismantling sophisticated fraud operations and restoring program integrity.
Implications and the Path Forward
Importance of Safeguarding Public Funds
The case emphasizes the importance of safeguarding taxpayer-funded programs like Medicaid from fraudulent exploitation. Authorities’ prompt action in this matter reinforces their commitment to maintaining the integrity of public health systems and ensuring that such funds are used for their intended purpose. This case serves as a potent reminder of the ongoing need for vigilance and robust regulatory measures to protect public resources.
Preventing such fraud in the future requires a concerted effort to enhance oversight and accountability mechanisms within healthcare programs. Implementing stricter auditing processes, improving transparency, and fostering a more collaborative environment between agencies can mitigate the risk of such fraudulent activities taking root. Additionally, educating the public and healthcare providers about fraud prevention plays an integral role in safeguarding these essential services.
The Ongoing Effort to Protect Public Programs
In a startling revelation, three individuals associated with Evergreen Recovery, Inc., a facility dedicated to drug and alcohol treatment, have been entangled in a massive Medicaid fraud and money laundering scheme. This scandal underscores the vulnerabilities plaguing our healthcare systems. From March 2018 to July 2024, the scheme thrived on deceptive tactics designed to manipulate Medicaid and other healthcare programs. These individuals orchestrated fraudulent billing for services that either were never rendered or did not meet the criteria for reimbursement.
The brazenness of their actions highlights a significant weakness in oversight and regulation within healthcare reimbursement frameworks. It’s particularly disheartening as institutions meant to provide genuine care are instead exploiting the system for financial gain. This case serves as a stern reminder of the necessity for stricter surveillance and more rigorous checks within Medicaid and other healthcare initiatives to protect public funds and ensure that they are used appropriately to serve those in need of legitimate care.